A recent study shows a program adapted from the U.K. is making a difference when it comes to patient recovery in Alberta hospitals.
End PJ Paralysis is currently offered at all Calgary adult hospitals, along with several Edmonton zone hospitals and High River Hospital. It aims to get patients out of bed, dressed in their own clothes and moving as much as possible.
“In a gown, you feel like you’re sick, like you’re a patient. Getting dressed is a step in the right direction,” said Karl Sawatzky, who is currently a patient in the program in Calgary.
Health-care professionals have long recognized the negative physical and psychological effects of spending too much time in bed.
Some of the physical side effects include delirium, pneumonia, pressure injuries and overall weakness. Depression and lethargy are common psychological side effects.
Since 2019, End PJ Paralysis has been offered at the post-acute rehab unit at Foothills Medical Centre. The ward consists mainly of patients recovering from spinal cord, stroke or brain injury.
Patients are first encouraged to get out of bed and wash their own face or have a shower. The next step involves dressing themselves in their own clothes.
“You see how much better they feel,” Jill Congram, a nurse clinician with the program at the Foothills, said. “Part of healing is starting to feel good again.”
Bill Bennett, who had spinal surgery in April, is participating in the Foothills program.
“I used to have to call in nurses to turn me every couple of hours. Now I can get out of bed myself,” he said.
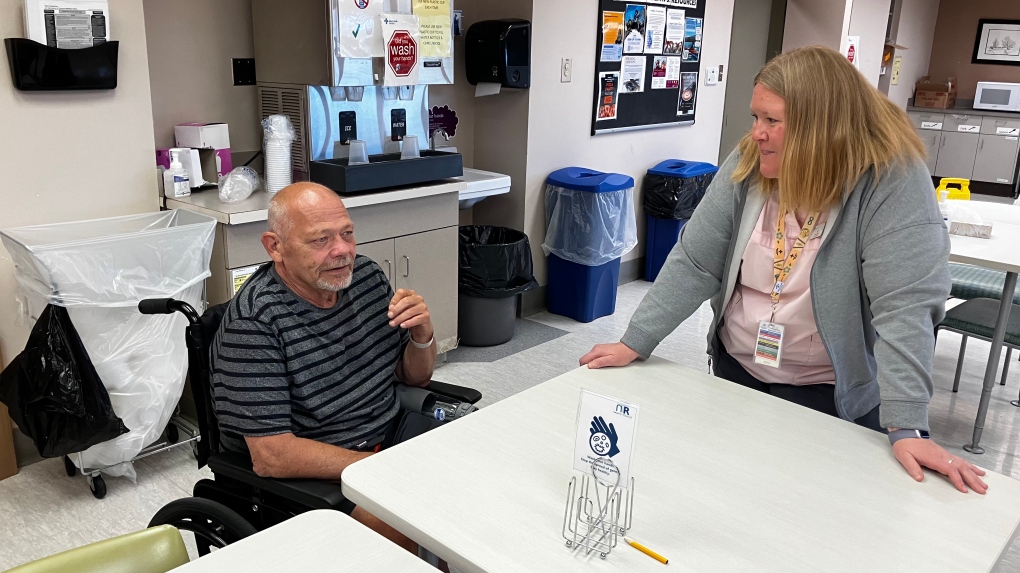 Bill Bennett, left, has been at Foothills Medical Center for more than three months after undergoing spinal surgery. (Courtesy: Alberta Health Services)
Bill Bennett, left, has been at Foothills Medical Center for more than three months after undergoing spinal surgery. (Courtesy: Alberta Health Services)
The small steps encouraged through the program are having an impact.
In April 2024, a study published in the Disability and Rehabilitation journal about the End PJ Paralysis outcomes at participating Alberta hospitals looked at the discharge data for 32,884 patients.
It found those in the program reduced their stay in hospital by 1.8 days.
The research also shows getting patients up and moving does not increase the risk of falling. In fact, it proved the opposite, that patients participating in the program had 2.2 fewer falls during their hospital stay.
And over time, the percentage of patients discharged to their homes, as opposed to long-term care facilities, increased. Mobilization and dressed rates also improved.
Sawatzky was diagnosed with Guillain-Barre syndrome in January. He spent two months in ICU at Foothills and one month in acute care. During that time, he got pneumonia five times.
Sawatzky says since being transferred to the post-acute rehab unit and taking part in the program, he hasn’t had pneumonia.
“It’s a night and day difference from then until now,” says Sawatzky. “Everything is coming back a lot faster. I wasn’t sure I would walk again. I was given a two-year recovery and in five months I’m already using a walker.”
While the program may sound simple, it’s not easy for the participants. “It’s difficult, challenging, it’s fatiguing,” says Congram.
She pointed out nurses have to balance their role between doing everything for the patient and being cheerleaders. They adapt based on a patient’s situation and abilities.
Bennett says he was eager to get up and moving but the encouragement to socialize has made the biggest difference.
Eating meals in the “cafeteria, was one of the best things for that. I’ve made friends that I will have for life,” he said.
Pandemic impact
The program hadn’t been running for long before the pandemic hit, and it had an impact.
“Momentum was lost during the COVID years,” says Paul Wright, the executive director for Calgary zone integrated quality management.
The 2024 study looked at the pandemic interruptions to the program and concluded there was a general reversal in the prior outcome gains.
There was a slight increase in the length of stay and inpatient fall rates. There was also a significant decline in the number of people discharged home.
Wright said there are several important factors contributing to the outcome decline. Restricted visitor numbers limited the amount of clothing and personal items being brought to patients.
Protective equipment to prevent the spread of the virus made socializing difficult. And there were limited areas for walking in the hospital.
“In the last four months, we have had a lot of energy around re-engaging the messages of getting patients up dressed and moving for better health in Calgary and in Edmonton,” Wright said.
Expanding the program
The 2024 study points out the growing need for more programs like End PJ Paralysis. It calls hospital immobility endemic in Canada and says it will only get worse with an aging population.
In Alberta, a plan is already underway to expand End PJ Paralysis into the community.
“I met with teams in the community and home care to see how we can spread the initiative to support patients in their own environment,” Wright said, adding he’s also recently spoken to and had education sessions with some Ontario-based hospitals looking to launch the program.